Narciso F. Atienza, Jr. MD, MBA, DPBO
EYE PHYSICIAN AND SURGEON
DIPLOMATE, PHILIPPINE BOARD OF OPHTHALMOLOGY
SUBSPECIALTY IN DISEASES AND SURGERY OF THE RETINA, VITREOUS, AND MACULA and OCULAR ONCOLOGY
DIPLOMATE, PHILIPPINE BOARD OF OPHTHALMOLOGY
SUBSPECIALTY IN DISEASES AND SURGERY OF THE RETINA, VITREOUS, AND MACULA and OCULAR ONCOLOGY

What is a cataract?
A cataract is a clouding of the normally clear lens of the eye. It can be compared to a window that is frosted or yellowed.
There are many misconceptions about cataract. Cataract is not:
A film over the eye;
Caused by overusing the eyes;
Spread from one eye to the other;
A cause of irreversible blindness.
What are the common symptoms of cataract?
A painless blurring of vision;
Glare, or light sensitivity;
Poor night vision;
Double vision in one eye;
Needing brighter light to read;
Fading or yellowing of colors.
The amount and pattern of cloudiness within the lens can vary. If the cloudiness is not near the center of the lens, you may not be aware that a cataract is present.
What causes cataract?
The most common type of cataract is related to aging of the eye. Causes of cataract include:
family history;
medical problems, such as diabetes;
injury to the eye;
medications, especially steroids;
long-term, unprotected exposure to sunlight;
previous eye surgery;
unknown factors.
How is a cataract detected?
Ophthalmologists have been expertly trained to diagnose and treat cataracts and other eye diseases. A thorough eye exam will determine whether cataracts are causing the symptoms.
This exam will include a visual acuity test, during which you will be asked to read an eye chart to assess what you are able to see. During a refraction test, different lenses will be placed in front of your eye to determine if a simple change in glasses can correct the problem.
The front of the eye will be examined using a slit lamp, a microscope that the doctor a magnified view of the eye. The slit lamp is also used to determine if cloudy vision is due to a problem with the cornea or other structures in front of the lens.
Finally the back of the eye will be examined using various instruments. Your doctor usually places dilating drops to do a very careful examination on the retina and optic nerve, to rule out other eye diseases causing the blurred vision. One such disease is age related macular degeneration (ARMD), which is a change in the retina due to aging and ARMD is the most common cause of a permanent vision loss in North America.
After the exam, the eye doctor will explain the cause of your blurred vision and discuss possible treatments.
How fast does a cataract develop?
How quickly the cataract develops varies among individuals, and may even be different between the two eyes. Most age-related cataracts progress gradually over a period of years.
Other cataracts, especially in younger people and people with diabetes, may progress rapidly over a short time. It is not possible to predict exactly how fast cataracts will develop in any given person.
Are there any medications I can take to prevent or reverse cataracts?
There is NO MEDICATION for cataract. Some eye doctors may prescribe drops that they claim that may help treat or delay the progression of cataracts. Even though some patients, especially those in the elderly with dry eye symptoms, would state an improvement in their sensation of their eyes or "vision" with the use of some of this drops, it is mostly attributed to the effect on the drops on the ocular tear film, which may smoothen out the eye surface. It doesn't affect the lens as this medications do not penetrate the eye to have an effect inside. Randomized clinical trials have shown that in patients who used the drops, their is NO DIFFERENCE on rate of cataract progression on patients who received the real drops from placebo.
What it the treatment for cataracts?
Cataract surgery involves removing the cloudy lens, from the eye and replacing it with a clear plastic lens. It is one of the most common operations performed in the Phillipines today. Cataract surgery in the Philippines is well in world standard of eye care and entails the use of cutting edge technology present in countries such as the United States and in Europe. Many Filipino ophthalmic surgeons offering this services ranks with the best of the world in terms of skill and equipment.
The cataract has the shape of a small magnifying lens and is about the size of the nail on your little finger (approximately 13 mm). The lens of the eye is covered by a very fine, thin, clear membrane lens capsule. The lens capsule is attached to the inside of the eye, just behind the iris by very fine attachments known as zonules. These zonules hold the lens in place and control its ability to focus.
Inside the capsule, the lens material is made of two components: soft material called the cortex and harder central material called the nucleus. In many ways, the lens of the eye is like a peach or cherry; the outside skin is the capsule, the pulp is the cortex and the pit is the nucleus.
Are there different types of cataract surgery?
There are a number of ways the cataract can be removed. These include:
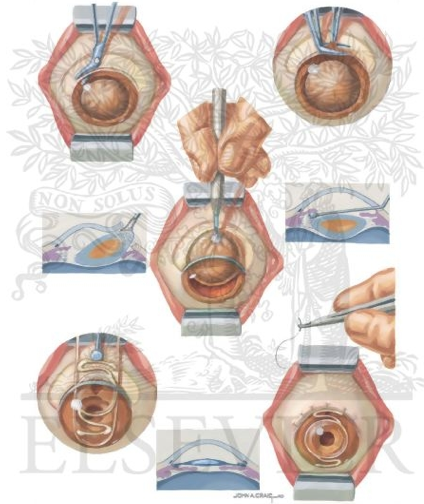
1) Intra-Capsular Cataract Extraction
Commonly used 30 years ago, intra-capsular cataract extraction, or ICCE, involved removing the lens, the entire lens capsule and its attachments from the eye. Patients were admitted to hospital for bed rest for approximately one week.
Because this technique was used before replacement lenses became available, the lens that was removed was not replaced. To see clearly after surgery, very thick glasses with a large magnifying effect (conmmonly known as "coke bottle" glasses) or anterior chamber lenses were used.
These glasses were difficult to get used to, many people had problems moving about, especially on uneven surfaces and or in new areas. Following surgery, patients had to lay still in bed while the eye healed, often with sandbags around their head to keep them from moving. With the development of better sutures (stitches), patients were released after a few days and their activities were less restricted.
2) Extra-Capsular Cataract Extraction
Extra-capsular cataract extraction (ECCE) refers to surgery in which the entire cataract is removed through a small hole made in the lens capsule. The rest of the lens capsule and all its attachments are left intact.
Most cataracts have a diameter of at least 10 mm. Therefore, an incision (cut) of at least this length has to be made to remove the cataract. The new lens, usually a PC IOL, is then placed in the lens capsule. At the end of the procedure, many tiny sutures (stitches) are needed to close the wound.
This procedure became very successful because patients could have surgery and go home the same day. However, because of the large incision, this procedure caused more problems than other modern surgical techniques. Many patients took longer to heal and to regain the ability to carry out daily activities. Eventually, a new procedure that reduced the size of the incision was developed.
These two techniques are not used much anymore except in special cases when phacoemulsification cannot be performed.
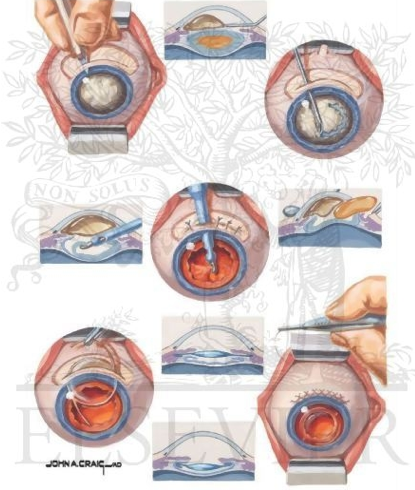
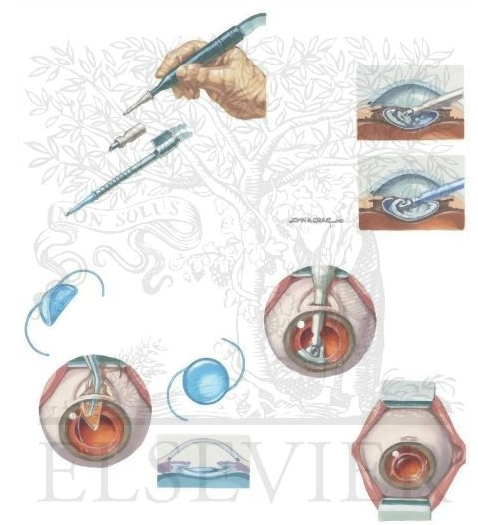
3) Phacoemulsification
Phacoemulsification removes the nucleus through a much smaller wound, and requires fewer or no sutures. This is the most popular method of cataract surgery in North America and Europe, and is the method employed by myself in 99% of cases.
Phacoemulsification machines use high frequency sound waves (ultrasound) to liquefy the contents of the lens, which can then be safely removed from the eye using suction through a 3 mm incision. There are other eye MD's which claim that they use LASER to dissolve the cataract. This claims of doctors using machines to remove the cataract completely are FALSE as these LASER ASSISTED CATARACT SURGERY MACHINES are NOT WIDELY AVAILABLE in the Philippines, and would still need ultrasound to remove the cataract. Furthermore, laser machines have been found not to be suitable for dense cataracts, which are found in Filipinos. The only available widely used laser for cataract surgery worldwide is for secondary cataract using a YAG laser, which is usually done in the office and NOT in the operating room.
Smaller incisions mean safer surgery because the surgeon can control eye pressure during surgery. Smaller wounds also heal faster and patients can return to normal life more quickly.
Surgery using the phacoemulsifier and a foldable lens can be done through an incision of about 2.5mm. This technique is much safer, making complications during or after surgery much less likely. Patients enjoy increased freedom, as they are able to move around immediately after surgery, and tend to recover more quickly.
What are some of the risks and possible complications of cataract surgery?
Cataract surgery is one of the safest surgeries performed in medicine today. However, it is important to remember that any operation carries the risk of complications. These complications can be divided into two categories: major (very serious) and minor.
Major complications may include:
- Endophthalmitis (severe infection inside the eye)
- Suprachoroidal Hemorrhage (severe bleeding inside the eye)
- Bullous Keratopathy (swelling of the cornea that cannot be reversed)
- Retinal Detachment
Minor Complications may include:
- An irregular pupil shape
- Iritis, inflammation or swelling inside the eye
- Off-centre lens placement
- Retinal tear or retinal hole
- Glaucoma, raised internal eye pressure
- Macular Edema, swelling of the central retina
- Secondary Cataract
Thanks to new surgical techniques, most of these complications occur very rarely. When they do start, most are very treatable.
The most serious complication is a bacterial infection inside the eye endophthalmitis. This type of infection can lead to loss of sight or even loss of the eye itself. It affects only one of every few thousand patients, despite the many precautions that are taken such as using sterile instruments, giving antibiotics before and after surgery, and sterilizing the eye before surgery.
Secondary Cataract
Up to 30 percent of patients develop a clouding of the back of the capsular bag after surgery, usually within a few months or a few years.
This clouding occurs as a result of cells moving onto this part of the capsule. It is easily treated with a YAG laser, which allows the surgeon to make a hole in the cloudy capsule and clear the vision. This simple office procedure takes only a few minutes to complete. Its most common complications include:
- Glaucoma, elevated internal eye pressure
- Retinal tear or detachment
- Inflammation or swelling
After the YAG procedure, your doctor will arrange a follow-up visit and provide drops to control the pressure inside the eye and swelling.
It is important to note that the first cataract is always removed using one of the traditional surgeries. Only secondary cataracts that developed after surgery can be removed by laser.
A cataract is a clouding of the normally clear lens of the eye. It can be compared to a window that is frosted or yellowed.
There are many misconceptions about cataract. Cataract is not:
A film over the eye;
Caused by overusing the eyes;
Spread from one eye to the other;
A cause of irreversible blindness.
What are the common symptoms of cataract?
A painless blurring of vision;
Glare, or light sensitivity;
Poor night vision;
Double vision in one eye;
Needing brighter light to read;
Fading or yellowing of colors.
The amount and pattern of cloudiness within the lens can vary. If the cloudiness is not near the center of the lens, you may not be aware that a cataract is present.
What causes cataract?
The most common type of cataract is related to aging of the eye. Causes of cataract include:
family history;
medical problems, such as diabetes;
injury to the eye;
medications, especially steroids;
long-term, unprotected exposure to sunlight;
previous eye surgery;
unknown factors.
How is a cataract detected?
Ophthalmologists have been expertly trained to diagnose and treat cataracts and other eye diseases. A thorough eye exam will determine whether cataracts are causing the symptoms.
This exam will include a visual acuity test, during which you will be asked to read an eye chart to assess what you are able to see. During a refraction test, different lenses will be placed in front of your eye to determine if a simple change in glasses can correct the problem.
The front of the eye will be examined using a slit lamp, a microscope that the doctor a magnified view of the eye. The slit lamp is also used to determine if cloudy vision is due to a problem with the cornea or other structures in front of the lens.
Finally the back of the eye will be examined using various instruments. Your doctor usually places dilating drops to do a very careful examination on the retina and optic nerve, to rule out other eye diseases causing the blurred vision. One such disease is age related macular degeneration (ARMD), which is a change in the retina due to aging and ARMD is the most common cause of a permanent vision loss in North America.
After the exam, the eye doctor will explain the cause of your blurred vision and discuss possible treatments.
How fast does a cataract develop?
How quickly the cataract develops varies among individuals, and may even be different between the two eyes. Most age-related cataracts progress gradually over a period of years.
Other cataracts, especially in younger people and people with diabetes, may progress rapidly over a short time. It is not possible to predict exactly how fast cataracts will develop in any given person.
Are there any medications I can take to prevent or reverse cataracts?
There is NO MEDICATION for cataract. Some eye doctors may prescribe drops that they claim that may help treat or delay the progression of cataracts. Even though some patients, especially those in the elderly with dry eye symptoms, would state an improvement in their sensation of their eyes or "vision" with the use of some of this drops, it is mostly attributed to the effect on the drops on the ocular tear film, which may smoothen out the eye surface. It doesn't affect the lens as this medications do not penetrate the eye to have an effect inside. Randomized clinical trials have shown that in patients who used the drops, their is NO DIFFERENCE on rate of cataract progression on patients who received the real drops from placebo.
What it the treatment for cataracts?
Cataract surgery involves removing the cloudy lens, from the eye and replacing it with a clear plastic lens. It is one of the most common operations performed in the Phillipines today. Cataract surgery in the Philippines is well in world standard of eye care and entails the use of cutting edge technology present in countries such as the United States and in Europe. Many Filipino ophthalmic surgeons offering this services ranks with the best of the world in terms of skill and equipment.
The cataract has the shape of a small magnifying lens and is about the size of the nail on your little finger (approximately 13 mm). The lens of the eye is covered by a very fine, thin, clear membrane lens capsule. The lens capsule is attached to the inside of the eye, just behind the iris by very fine attachments known as zonules. These zonules hold the lens in place and control its ability to focus.
Inside the capsule, the lens material is made of two components: soft material called the cortex and harder central material called the nucleus. In many ways, the lens of the eye is like a peach or cherry; the outside skin is the capsule, the pulp is the cortex and the pit is the nucleus.
Are there different types of cataract surgery?
There are a number of ways the cataract can be removed. These include:
1) Intra-Capsular Cataract Extraction
Commonly used 30 years ago, intra-capsular cataract extraction, or ICCE, involved removing the lens, the entire lens capsule and its attachments from the eye. Patients were admitted to hospital for bed rest for approximately one week.
Because this technique was used before replacement lenses became available, the lens that was removed was not replaced. To see clearly after surgery, very thick glasses with a large magnifying effect (conmmonly known as "coke bottle" glasses) or anterior chamber lenses were used.
These glasses were difficult to get used to, many people had problems moving about, especially on uneven surfaces and or in new areas. Following surgery, patients had to lay still in bed while the eye healed, often with sandbags around their head to keep them from moving. With the development of better sutures (stitches), patients were released after a few days and their activities were less restricted.
2) Extra-Capsular Cataract Extraction
Extra-capsular cataract extraction (ECCE) refers to surgery in which the entire cataract is removed through a small hole made in the lens capsule. The rest of the lens capsule and all its attachments are left intact.
Most cataracts have a diameter of at least 10 mm. Therefore, an incision (cut) of at least this length has to be made to remove the cataract. The new lens, usually a PC IOL, is then placed in the lens capsule. At the end of the procedure, many tiny sutures (stitches) are needed to close the wound.
This procedure became very successful because patients could have surgery and go home the same day. However, because of the large incision, this procedure caused more problems than other modern surgical techniques. Many patients took longer to heal and to regain the ability to carry out daily activities. Eventually, a new procedure that reduced the size of the incision was developed.
These two techniques are not used much anymore except in special cases when phacoemulsification cannot be performed.
3) Phacoemulsification
Phacoemulsification removes the nucleus through a much smaller wound, and requires fewer or no sutures. This is the most popular method of cataract surgery in North America and Europe, and is the method employed by myself in 99% of cases.
Phacoemulsification machines use high frequency sound waves (ultrasound) to liquefy the contents of the lens, which can then be safely removed from the eye using suction through a 3 mm incision. There are other eye MD's which claim that they use LASER to dissolve the cataract. This claims of doctors using machines to remove the cataract completely are FALSE as these LASER ASSISTED CATARACT SURGERY MACHINES are NOT WIDELY AVAILABLE in the Philippines, and would still need ultrasound to remove the cataract. Furthermore, laser machines have been found not to be suitable for dense cataracts, which are found in Filipinos. The only available widely used laser for cataract surgery worldwide is for secondary cataract using a YAG laser, which is usually done in the office and NOT in the operating room.
Smaller incisions mean safer surgery because the surgeon can control eye pressure during surgery. Smaller wounds also heal faster and patients can return to normal life more quickly.
Surgery using the phacoemulsifier and a foldable lens can be done through an incision of about 2.5mm. This technique is much safer, making complications during or after surgery much less likely. Patients enjoy increased freedom, as they are able to move around immediately after surgery, and tend to recover more quickly.
What are some of the risks and possible complications of cataract surgery?
Cataract surgery is one of the safest surgeries performed in medicine today. However, it is important to remember that any operation carries the risk of complications. These complications can be divided into two categories: major (very serious) and minor.
Major complications may include:
- Endophthalmitis (severe infection inside the eye)
- Suprachoroidal Hemorrhage (severe bleeding inside the eye)
- Bullous Keratopathy (swelling of the cornea that cannot be reversed)
- Retinal Detachment
Minor Complications may include:
- An irregular pupil shape
- Iritis, inflammation or swelling inside the eye
- Off-centre lens placement
- Retinal tear or retinal hole
- Glaucoma, raised internal eye pressure
- Macular Edema, swelling of the central retina
- Secondary Cataract
Thanks to new surgical techniques, most of these complications occur very rarely. When they do start, most are very treatable.
The most serious complication is a bacterial infection inside the eye endophthalmitis. This type of infection can lead to loss of sight or even loss of the eye itself. It affects only one of every few thousand patients, despite the many precautions that are taken such as using sterile instruments, giving antibiotics before and after surgery, and sterilizing the eye before surgery.
Secondary Cataract
Up to 30 percent of patients develop a clouding of the back of the capsular bag after surgery, usually within a few months or a few years.
This clouding occurs as a result of cells moving onto this part of the capsule. It is easily treated with a YAG laser, which allows the surgeon to make a hole in the cloudy capsule and clear the vision. This simple office procedure takes only a few minutes to complete. Its most common complications include:
- Glaucoma, elevated internal eye pressure
- Retinal tear or detachment
- Inflammation or swelling
After the YAG procedure, your doctor will arrange a follow-up visit and provide drops to control the pressure inside the eye and swelling.
It is important to note that the first cataract is always removed using one of the traditional surgeries. Only secondary cataracts that developed after surgery can be removed by laser.