Narciso F. Atienza, Jr. MD, MBA, DPBO
EYE PHYSICIAN AND SURGEON
DIPLOMATE, PHILIPPINE BOARD OF OPHTHALMOLOGY
SUBSPECIALTY IN DISEASES AND SURGERY OF THE RETINA, VITREOUS, AND MACULA and OCULAR ONCOLOGY
DIPLOMATE, PHILIPPINE BOARD OF OPHTHALMOLOGY
SUBSPECIALTY IN DISEASES AND SURGERY OF THE RETINA, VITREOUS, AND MACULA and OCULAR ONCOLOGY

What is a retinal detachment?
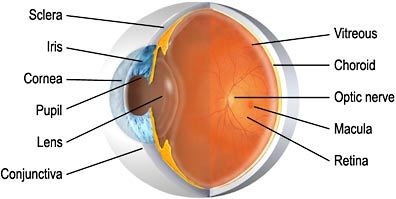
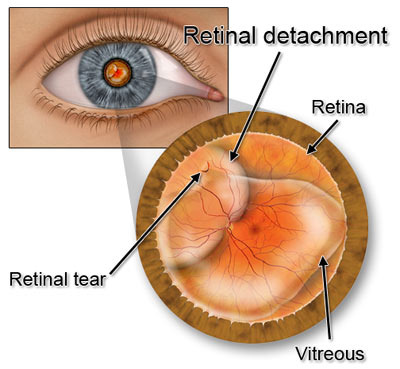
A retinal detachment is the separation of the retina from its attachment from the choroid. This occurs when the light sensitive layer at the back of the eye, the retina, separates from the wall of the eye due to a tear or multiple tears in the retina. The symptoms of a retinal detachment can include floaters, flashes of light, a dark shadow blocking part of your view, or loss of central vision.
What causes retinal detachment?
Retinal detachment is caused by a combination of factors including retinal holes, retinal breaks, or retinal tears, liquefaction of the vitreous humor, and mechanical forces on the retina often referred to as “traction”. There are 3 general types of retinal detachment namely:
1) rhegmatogenous retinal detachment - caused by a torn retina or a retinal break caused by traction on retinal surface
2) exudative retinal detachment - caused by fluid accumulation underneath the retina
3) traction retinal detachment - cause by an extrinsic factor pulling on the retina, such as membranes. This detachment is not associated with the presence of a retinal break.
Rhegmatogenous and traction detachments are usually treated with surgery, while exudative detachments are treated by treating the primary cause.
What causes retinal holes, retinal breaks or retinal tears?
A variety of factors including:
1. Hereditary abnormalities of the peripheral retina often associated with myopia (near-sightedness)
2. eye trauma
3. complications of eye surgery for cataract or glaucoma
4. various retinal and macular diseases
5. vision correction.
What is the relationship between near-sightedness and retinal detachment?
Simply having a longer eye associated with myopia probably does not cause retinal detachment, tears, holes, or breaks. A variety of peripheral retinal degenerations such as lattice degeneration are often genetically linked to myopia and may cause retinal holes, breaks or tears.
If a retinal detachment occurs after eye surgery, does it mean that the surgeon made a mistake?
No. Retinal holes, breaks, or tears can occur after uncomplicated eye surgery performed at the highest level of skill and competence. This complication is probably related to normal alterations in the vitreous humor (jelly) that often occurs during or after surgery.
Can retinal detachment cause total blindness?
Yes, even a slight blockage of the vision caused by partial retinal detachment can result in blindness if not treated early.
How common is retinal detachment?
It is uncommon, happening in 1 out of 2000 to 5000 patients.
Are eye strain, nutrition, general health, smoking, or emotional stress related to retinal detachment?
No. There is no known relationship between retinal detachment and any of these problems.
Is there a medication or eye drop for the treatment for retinal detachment or is surgery the only option?
No, there is no medicine, eye drop, vitamin, herb, or diet that is beneficial to patients with retinal detachment. Surgery is the only option.
How is retinal detachment treated?
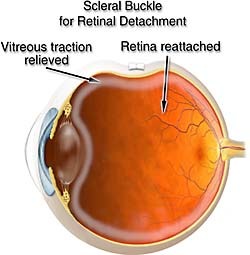
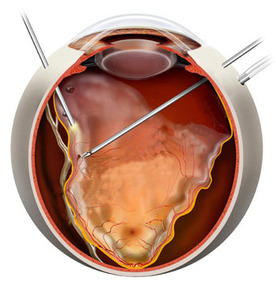
Your regular ophthalmologist will refer you to a retina surgeon (an ophthalmologist who has undergone at least one year in clinical fellowship in retinal surgery, and is practicing fulltime in this subspecialty) to manage your retinal detachment. Your retinal surgeon will discuss the treatment options for your retinal detachment whether he will do laser, scleral buckle, a vitrectomy, to use a special inert gas, or silicone oil, or a combination to treat your retinal detachment. Your retinal surgeon will recommend what is best to try to treat your condition.
Are there complications and is the surgery always successful?
There is always a small chance of complications after surgery. Among them are:
• Infection
• Bleeding
• Recurrent retinal detachment
• High pressure in the eye
• Some loss of side vision
• Accelerated cataract formation
This risk occurs in a very low rate, that the surgery is more in favor for patients. Without surgery, the risk of total blindness from retinal detachment goes almost 100%. Surgery may not be successful in one sitting, so there are occasions that surgery has to be staged or repeated to repair the retinal detachment. At, most, the success rate for a single surgery is around 85%, depending on 1) how severe and how long your retinal detachment has been present, and 2) how experienced your retinal surgeon is. The longer the detachment has been present and more severe it is on presentation, the more extensive surgery and the lower success rate it has after surgery.
Despite a successful surgery, vision recovery may not be optimal as micro-damage on the retina usually occurs at the onset of retinal detachment. This is the reason why retinal detachments are repaired with urgency, so as to limit this damage. There will be precautions after the surgery, and your retina surgeon will discuss these with you prior to surgery
A retinal detachment is the separation of the retina from its attachment from the choroid. This occurs when the light sensitive layer at the back of the eye, the retina, separates from the wall of the eye due to a tear or multiple tears in the retina. The symptoms of a retinal detachment can include floaters, flashes of light, a dark shadow blocking part of your view, or loss of central vision.
What causes retinal detachment?
Retinal detachment is caused by a combination of factors including retinal holes, retinal breaks, or retinal tears, liquefaction of the vitreous humor, and mechanical forces on the retina often referred to as “traction”. There are 3 general types of retinal detachment namely:
1) rhegmatogenous retinal detachment - caused by a torn retina or a retinal break caused by traction on retinal surface
2) exudative retinal detachment - caused by fluid accumulation underneath the retina
3) traction retinal detachment - cause by an extrinsic factor pulling on the retina, such as membranes. This detachment is not associated with the presence of a retinal break.
Rhegmatogenous and traction detachments are usually treated with surgery, while exudative detachments are treated by treating the primary cause.
What causes retinal holes, retinal breaks or retinal tears?
A variety of factors including:
1. Hereditary abnormalities of the peripheral retina often associated with myopia (near-sightedness)
2. eye trauma
3. complications of eye surgery for cataract or glaucoma
4. various retinal and macular diseases
5. vision correction.
What is the relationship between near-sightedness and retinal detachment?
Simply having a longer eye associated with myopia probably does not cause retinal detachment, tears, holes, or breaks. A variety of peripheral retinal degenerations such as lattice degeneration are often genetically linked to myopia and may cause retinal holes, breaks or tears.
If a retinal detachment occurs after eye surgery, does it mean that the surgeon made a mistake?
No. Retinal holes, breaks, or tears can occur after uncomplicated eye surgery performed at the highest level of skill and competence. This complication is probably related to normal alterations in the vitreous humor (jelly) that often occurs during or after surgery.
Can retinal detachment cause total blindness?
Yes, even a slight blockage of the vision caused by partial retinal detachment can result in blindness if not treated early.
How common is retinal detachment?
It is uncommon, happening in 1 out of 2000 to 5000 patients.
Are eye strain, nutrition, general health, smoking, or emotional stress related to retinal detachment?
No. There is no known relationship between retinal detachment and any of these problems.
Is there a medication or eye drop for the treatment for retinal detachment or is surgery the only option?
No, there is no medicine, eye drop, vitamin, herb, or diet that is beneficial to patients with retinal detachment. Surgery is the only option.
How is retinal detachment treated?
Your regular ophthalmologist will refer you to a retina surgeon (an ophthalmologist who has undergone at least one year in clinical fellowship in retinal surgery, and is practicing fulltime in this subspecialty) to manage your retinal detachment. Your retinal surgeon will discuss the treatment options for your retinal detachment whether he will do laser, scleral buckle, a vitrectomy, to use a special inert gas, or silicone oil, or a combination to treat your retinal detachment. Your retinal surgeon will recommend what is best to try to treat your condition.
Are there complications and is the surgery always successful?
There is always a small chance of complications after surgery. Among them are:
• Infection
• Bleeding
• Recurrent retinal detachment
• High pressure in the eye
• Some loss of side vision
• Accelerated cataract formation
This risk occurs in a very low rate, that the surgery is more in favor for patients. Without surgery, the risk of total blindness from retinal detachment goes almost 100%. Surgery may not be successful in one sitting, so there are occasions that surgery has to be staged or repeated to repair the retinal detachment. At, most, the success rate for a single surgery is around 85%, depending on 1) how severe and how long your retinal detachment has been present, and 2) how experienced your retinal surgeon is. The longer the detachment has been present and more severe it is on presentation, the more extensive surgery and the lower success rate it has after surgery.
Despite a successful surgery, vision recovery may not be optimal as micro-damage on the retina usually occurs at the onset of retinal detachment. This is the reason why retinal detachments are repaired with urgency, so as to limit this damage. There will be precautions after the surgery, and your retina surgeon will discuss these with you prior to surgery