Narciso F. Atienza, Jr. MD, MBA, DPBO
EYE PHYSICIAN AND SURGEON
DIPLOMATE, PHILIPPINE BOARD OF OPHTHALMOLOGY
SUBSPECIALTY IN DISEASES AND SURGERY OF THE RETINA, VITREOUS, AND MACULA and OCULAR ONCOLOGY
DIPLOMATE, PHILIPPINE BOARD OF OPHTHALMOLOGY
SUBSPECIALTY IN DISEASES AND SURGERY OF THE RETINA, VITREOUS, AND MACULA and OCULAR ONCOLOGY

What is Diabetic Eye Disease?
Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of this disease. All can cause severe vision loss or even blindness. Diabetic eye disease may include:
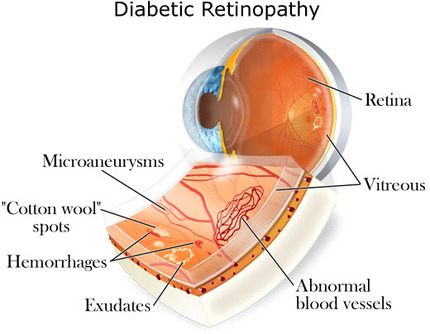
Diabetic Retinopathy – damage to the blood vessels in the retina.
Cataracts – clouding of the eye’s lens
Glaucoma – increase in fluid pressure inside the eye that leads to optic nerve damage and loss of vision.
Cataracts and glaucoma also affect many people who do not have diabetes.
What is the most common diabetic eye disease?
Diabetic retinopathy. This disease is a leading cause of preventable blindness in Filipino adults. It is cause by changes in the blood vessels of the retina. In some people with diabetic retinopathy, retinal blood vessels may swell and leak fluid. In other people, abnormal new blood vessels grow on the surface of the retina. These changes may result in vision loss or blindness.
Who is most likely to get diabetic retinopathy?
Anyone with diabetes. The longer someone has diabetes, the more likely he/she will get diabetic retinopathy. Nearly half of all people with diabetes will develop some degree of diabetic retinopathy during their lifetime.
What are its’ symptoms?
Often there are none in the early stages of the disease. Visual acuity may not change until the disease becomes severe and is usually painless.
Blurred vision may occur when the macula—the part of the retina that provides sharp central vision, swells from the leaking fluid. This condition is called macular edema. If new vessels have grown on the surface of the retina, they can bleed into the eye, blocking vision. But, even in more advanced cases, the disease may progress a long way without symptoms. That is why regular eye examinations for people with diabetes are so important.
If you have diabetes, you should have your eyes examined at least every six months by a competent ophthalmologist, preferably a retina specialist. Your eyes should be dilated during the examination. That means eyedrops are used to enlarge your pupils, This allows the eye doctor to see more of the inside of your eyes to check for signs of the disease using special equipment such as an indirect ophthalmoscope.
How do we treat diabetic retinopathy?
No medications have been proven to control or reduce the risks of diabetic retinopathy. Controlling your blood sugar, together with controlling your cholesterol levels, and blood pressure, is the mainstay for preventing and managing diabetic complications.
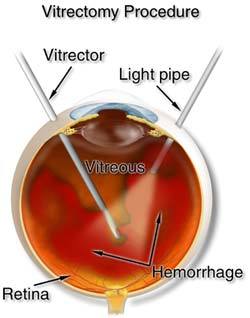
Depending on the stage of retinopathy, your eye doctor may suggest observation, laser surgery, an eye injection, vitrectomy surgery or a combination.
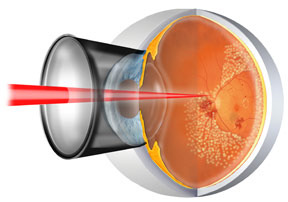
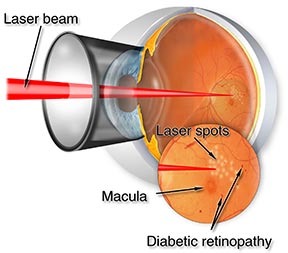
Laser is a strong light beam aimed at the retina to seal leaking vessels in case of macular edema or to shrink abnormal vessels in cases of proliferative retinopathy. Laser surgery has been proven to reduce the risk of severe vision loss in proliferative disease by 60-70%. In cases of macular edema, laser often cannot restore vision that has already been lost, but it is often done to limit the amount of damage done. That is why finding diabetic retinopathy early is the best way to prevent vision loss.
Recently, anti-VEGF (Vascular Endothelial Growth Factor) antibodies have been used to treat diabetic retinopathy. This injections can control the amount of swelling or bleeding but will have to be administered for a very long period of time to control or halt diabetic retinopathy. Most of the use of anti-VEGF is for pre-operative surgical adjunct to reduce the amount of bleeding during surgery. Laser or surgery is still the best way to halt the progression, together with strict blood sugar, blood pressure, and cholesterol control.
Cataract surgery performed if you have advanced diabetic retinopathy will likely not cause any remarkable improvement, and it may also cause a worsening of your vision in the long run.
The Diabetes Control and Complications Trial (DCCT) showed that better control of blood sugar levels slows the onset and progression of retinopathy and lessens the need for laser surgery for severe retinopathy.
The study found that the group that tried to keep their blood sugar levels as close to normal as possible had much less eye, kidney, and nerve disease. This level of blood sugar control may not be best for everyone, including some elderly patients, children under 13 or people with heart disease. So ask your doctor if this program is right for you.
How common are the other diabetic eye diseases?
If you have diabetes, you are also at risk for other diabetic eye diseases. Studies show that you are twice as likely to get a cataract as a person compared to somebody who does not have the disease. Also, cataracts develop at an earlier age in people with diabetes. Cataracts are treated with surgery, if you have no or not too severe retinopathy. Diabetic retinopathy does not happen overnight as most patients with retinopathy have been diabetic for at least 10 years prior to the detection of the early signs of diabetic retinopathy.
Glaucoma may also become a problem. A person with diabetes is nearly twice as likely to get glaucoma as other adults. And, as with diabetic retinopathy, the longer you have had diabetes, the greater your risk of getting glaucoma. Glaucoma may be treated with medications, laser, or if very severe, other forms of eye surgery.
What can you do to protect your vision?
Finding and treating the disease early, before it causes vision loss or blindness, is the best way to control diabetic eye disease. So, if you have diabetes, make sure you get a dilated eye examination at least every 6 months.
Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of this disease. All can cause severe vision loss or even blindness. Diabetic eye disease may include:
Diabetic Retinopathy – damage to the blood vessels in the retina.
Cataracts – clouding of the eye’s lens
Glaucoma – increase in fluid pressure inside the eye that leads to optic nerve damage and loss of vision.
Cataracts and glaucoma also affect many people who do not have diabetes.
What is the most common diabetic eye disease?
Diabetic retinopathy. This disease is a leading cause of preventable blindness in Filipino adults. It is cause by changes in the blood vessels of the retina. In some people with diabetic retinopathy, retinal blood vessels may swell and leak fluid. In other people, abnormal new blood vessels grow on the surface of the retina. These changes may result in vision loss or blindness.
Who is most likely to get diabetic retinopathy?
Anyone with diabetes. The longer someone has diabetes, the more likely he/she will get diabetic retinopathy. Nearly half of all people with diabetes will develop some degree of diabetic retinopathy during their lifetime.
What are its’ symptoms?
Often there are none in the early stages of the disease. Visual acuity may not change until the disease becomes severe and is usually painless.
Blurred vision may occur when the macula—the part of the retina that provides sharp central vision, swells from the leaking fluid. This condition is called macular edema. If new vessels have grown on the surface of the retina, they can bleed into the eye, blocking vision. But, even in more advanced cases, the disease may progress a long way without symptoms. That is why regular eye examinations for people with diabetes are so important.
If you have diabetes, you should have your eyes examined at least every six months by a competent ophthalmologist, preferably a retina specialist. Your eyes should be dilated during the examination. That means eyedrops are used to enlarge your pupils, This allows the eye doctor to see more of the inside of your eyes to check for signs of the disease using special equipment such as an indirect ophthalmoscope.
How do we treat diabetic retinopathy?
No medications have been proven to control or reduce the risks of diabetic retinopathy. Controlling your blood sugar, together with controlling your cholesterol levels, and blood pressure, is the mainstay for preventing and managing diabetic complications.
Depending on the stage of retinopathy, your eye doctor may suggest observation, laser surgery, an eye injection, vitrectomy surgery or a combination.
Laser is a strong light beam aimed at the retina to seal leaking vessels in case of macular edema or to shrink abnormal vessels in cases of proliferative retinopathy. Laser surgery has been proven to reduce the risk of severe vision loss in proliferative disease by 60-70%. In cases of macular edema, laser often cannot restore vision that has already been lost, but it is often done to limit the amount of damage done. That is why finding diabetic retinopathy early is the best way to prevent vision loss.
Recently, anti-VEGF (Vascular Endothelial Growth Factor) antibodies have been used to treat diabetic retinopathy. This injections can control the amount of swelling or bleeding but will have to be administered for a very long period of time to control or halt diabetic retinopathy. Most of the use of anti-VEGF is for pre-operative surgical adjunct to reduce the amount of bleeding during surgery. Laser or surgery is still the best way to halt the progression, together with strict blood sugar, blood pressure, and cholesterol control.
Cataract surgery performed if you have advanced diabetic retinopathy will likely not cause any remarkable improvement, and it may also cause a worsening of your vision in the long run.
The Diabetes Control and Complications Trial (DCCT) showed that better control of blood sugar levels slows the onset and progression of retinopathy and lessens the need for laser surgery for severe retinopathy.
The study found that the group that tried to keep their blood sugar levels as close to normal as possible had much less eye, kidney, and nerve disease. This level of blood sugar control may not be best for everyone, including some elderly patients, children under 13 or people with heart disease. So ask your doctor if this program is right for you.
How common are the other diabetic eye diseases?
If you have diabetes, you are also at risk for other diabetic eye diseases. Studies show that you are twice as likely to get a cataract as a person compared to somebody who does not have the disease. Also, cataracts develop at an earlier age in people with diabetes. Cataracts are treated with surgery, if you have no or not too severe retinopathy. Diabetic retinopathy does not happen overnight as most patients with retinopathy have been diabetic for at least 10 years prior to the detection of the early signs of diabetic retinopathy.
Glaucoma may also become a problem. A person with diabetes is nearly twice as likely to get glaucoma as other adults. And, as with diabetic retinopathy, the longer you have had diabetes, the greater your risk of getting glaucoma. Glaucoma may be treated with medications, laser, or if very severe, other forms of eye surgery.
What can you do to protect your vision?
Finding and treating the disease early, before it causes vision loss or blindness, is the best way to control diabetic eye disease. So, if you have diabetes, make sure you get a dilated eye examination at least every 6 months.